Dr. Dineo Khabele, Professor and Chair of the Department of Obstetrics & Gynecology at Washington University School of Medicine in St. Louis and member of OCRA’s Scientific Advisory Committee, spoke at our 2020 Ovarian Cancer National Conference about the racial disparities in ovarian cancer incidences and outcomes. While there are more documented cases of ovarian cancer in white patients, the outcomes for Black women are worse. Dr. Khabele began her presentation with a quote by Dr. Martin Luther King Jr.
“Of all the forms of inequality, injustice in healthcare is the most shocking and inhumane.”
Dr. Martin Luther King Jr.
Despite nearly 55 years passing since Dr. King made this declaration at the second convention of the Medical Committee for Human Rights in March 1966, we still see shocking inequities.
The 5-year ovarian cancer survival rate for white women is 46%; in Black patients, it’s 36%. A similar pattern exists with cervical and uterine cancer. At the time of this presentation, Black people were dying from Covid-19 at 2.5 times the rate of white people, and Black women are three times more likely to die from pregnancy complications than their white counterparts.
The list continues: Black patients are less likely to receive appropriate cardiac medication and undergo coronary artery bypass surgery; they are more likely to be diagnosed in late stages for breast cancer; and they are more likely to receive lower quality basic clinical services like intensive care.
This matters. It matters from a moral and ethical standpoint, and this inequity comes at a great economic cost to society. After all, it costs far less to reduce the risk of a disease than to treat it.
Tiers of racial inequity
Dr. Khabele spoke of three sets of factors that lead to the above inequities:
- Systemic (ie – geography; type of hospital; inadequate insurance policies)
- Physician (ie – low-volume surgeons in regional referral centers who don’t see enough cases; biased clinical decision making)
- Patient (i.e. – low socioeconomic communities are unreached and underserved; fear and mistrust of medical establishment)
Regarding the physician level of inequity, Dr. Khabele spoke of four myths that many medical professionals hold:
- Fibroid tumors are more common in Black women
- BRCA mutations are not common in Black women
- Black women are not willing to undergo treatment
- Black people have less sensitive nerve endings
To repeat, the above are myths. But if a physician submits to any of these untruths, whether consciously or unconsciously, it’s easy to see how this will impact getting a proper diagnosis and receiving quality treatment and care.
When it comes to patients themselves, the fear and distrust present in the Black community comes from a long and sordid history of mistreatment by the medical establishment. From the development of the speculum in 1840 and the surgeries performed on enslaved women without their consent and without anesthesia, to the decade’s long Tuskegee Study in the mid 1900’s that infected hundreds of men with syphilis, to the taking of cells without consent from a Black woman in 1951 in order to advance science. And if we want to lead ourselves to believe that this is the past and things are better now, one need only look at Serena Williams, who almost died after a C-section because doctors didn’t listen to her as she advocated for the needs of and feelings within her own body.
Righting the wrongs of racial inequity in healthcare
Dr. Khabele spoke of several ways to address these inequities. We must listen to Black women and believe their stories and their pain. We need to train more Black doctors, nurses and healthcare workers in order to better reflect the patient population. Only 32% of oncologists are women, and only 2.3% of practicing oncologists are Black. Only 7.8% of nurses are Black. And we have to do a lot more work at building trust within the communities we intend to serve, which begins with the recognition that both doctor and patient have expertise: doctors may have medical knowledge, but patients have self-knowledge of their own lived experience. And this needs to be heard.
Addressing these issues, Dr. Khabele says, is critical from a moral and economic standpoint. And in doing so, it will lead to better care for all of us.
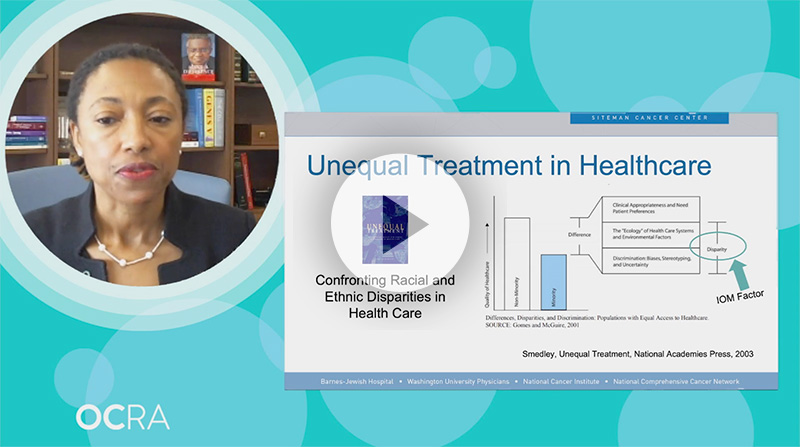
To learn more, you can watch Dr. Khabele’s presentation, Racial Disparities in Ovarian Cancer, from OCRA’s Ovarian Cancer National Conference.