Gynecologic Cancers
Recognizing the interconnectedness of ovarian and all gynecologic cancers, OCRA expanded its scope in order to accelerate research and broaden our impact on patients’ lives.
The most common gynecologic cancer, endometrial cancer develops from the inner lining of the uterus and is commonly referred to as uterine cancer.
To understand endometrial cancer, it’s important to learn about the different layers that make up the uterus.
The uterus is approximately the size and shape of a pear. The upper part of the uterus is the body, and is called the corpus. The lower part of the uterus, which rests just above the vagina, is the cervix.
The body (corpus) of the uterus consists of three layers, including:

OCRA’s online Clinical Trial Navigator is a simple, easy-to-use tool that helps you find clinical trials for endometrial cancer. Search by cancer type, treatment history, location and more.
While there is no screening test for endometrial cancer, many women are fortunately diagnosed at early stages because they have symptoms leading to an evaluation.
Endometrial cancer may be associated with some hereditary genetic syndromes such as Lynch syndrome (also called hereditary non-polyposis colon cancer syndrome or HNPCC), Cowden syndrome, or BRCA1 mutations. People with these genetic disorders may consider having yearly testing for endometrial cancer with a pelvic ultrasound and endometrial biopsy starting at age 35. The effectiveness of screening in these cases has not been established.
The most common symptom of endometrial cancer is abnormal bleeding. It is important to see a doctor if you experience abnorm
Several factors are linked to increased risk for endometrial cancer, including:
Several other factors are linked to decreased risk of developing endometrial cancer, including:
Endometrial cancer, also called endometrial carcinoma, is cancer that starts in the endometrium, the inner lining of the uterus. Most endometrial cancers are adenocarcinomas, which means they arise from glandular cells that line the uterine cavity. These cancers are subdivided into Type I and Type II tumors.
Type I tumors include endometrioid adenocarcinoma. These cancers often develop in response to high levels of estrogen and are typically diagnosed at early stages.
Type II tumors include less common subtypes such as serous adenocarcinoma or papillary serous adenocarcinoma. Clear cell carcinoma, carcinosarcoma, and undifferentiated carcinomas are included in this subset. Type II tumors classically do not develop in response to hormone signaling. These cancers may be more aggressive and are often diagnosed at later stages.
If you experience symptoms commonly associated with endometrial cancer, you should see your doctor, preferably a gynecologist. The gynecologist will perform a physical and a pelvic exam, and will discuss your symptoms, risk factors, and medical history.
A gynecologist may then perform an ultrasound to get a more detailed view of the uterus, ovaries, and fallopian tubes. Different types of ultrasounds may be performed. A pelvic ultrasound is a noninvasive procedure that can provide a clear picture of the abdomen, while a transvaginal ultrasound (TVUS) involves the insertion of a probe into the vagina, which can provide a clearer view of the uterus. A TVUS can reveal if tumors are present, or if the endometrium is thicker than normal (anything over 4mm), which can be a sign of endometrial cancer.
Recent data indicates that the current 4mm cutoff for endometrial thickness misses a significant amount of cancers, particularly in Black women, leading to potential disparities in outcomes. For this reason, current best practices include recommendations to perform a biopsy if symptoms persist, or even before getting a TVUS.
If an ultrasound reveals cause for concern, a doctor will collect a tissue sample from the endometrium for closer inspection in the lab. A tissue sample, viewed under a microscope, is the only way to diagnose endometrial cancer definitively.
In most cases, a doctor will begin with an endometrial biopsy. This procedure, which is especially accurate in post-menopausal patients, involves inserting a thin tube through the vagina into the uterus to collect a tissue sample. As part of the procedure, a doctor may also perform a hysteroscopy — insertion of a small telescope to help identify and collect samples from any areas of concern. A doctor may use a local anesthetic to alleviate any discomfort from the procedures.
If an endometrial biopsy does not provide a definitive result, or cannot be completed in the clinic, a doctor may perform a dilation and curettage (D&C). This outpatient procedure takes less than an hour and is typically performed in a surgical center so that additional anesthesia or sedation can be administered. In a D&C, a doctor will dilate the cervix and use an instrument to scrape tissue from inside the uterus, for further analysis. A D&C may also include a hysteroscopy. Patients may experience cramping or spotting after a D&C.
Once endometrial tissue is collected, it is examined under a microscope to confirm or rule out cancer. If cancer cells are found, further analysis will determine the specific cancer type, and the grade of disease. Some patients may benefit from genetic testing, which can reveal changes in genes or proteins that can help guide recommendations for the most effective treatments.
Endometrial cancer stage can vary from stage 1 (I) to stage 4 (IV), and is determined, for the most part, by how far the cancer has spread. This is often determined at the time of surgery. Lower stage disease means the cancer is only found in the uterus, whereas a higher stage means the cancer has spread.
Staging can be complicated to understand, but it is an important factor in guiding treatment. Patients should not hesitate to ask their medical team for clarification as to cancer stage, and what that means for their treatment and prognosis. Read more about endometrial cancer staging from the American Cancer Society.
The main treatment for endometrial cancer is typically surgery, which should be performed by a gynecologic oncologist. In this surgery, called a total hysterectomy, the doctor will remove the uterus and cervix. In most cases, this can be done with minimally invasive laparoscopic or robotic surgery. Minimally invasive surgery requires only small incisions in the abdomen, and the uterus is typically removed through the vagina. In some situations the uterus may need to be removed through an incision in the abdomen. In certain cases, the doctor may performa radical hysterectomy, removing additional tissue around the uterus, and the upper part of the vagina.
Doctors may also perform a bilateral salpingo-oophorectomy (BSO), which involves removing the fallopian tubes and both ovaries. In a pre-menopausal patient, removing both ovaries will result in surgical menopause. Patients age 45 and under may wish to discuss the possibility of keeping one or both ovaries intact in order to delay menopause if this is a safe option based on the findings at the time of surgery.
In addition, surgery may involve removing lymph nodes, which will then be tested to better determine the cancer’s surgical stage and spread.
For early stage endometrioid adenocarcinoma, surgery and close monitoring may be the only treatment needed. Depending on the stage, and specific type of cancer, additional treatments may be needed after surgery. These may include the following:
The most effective regimen will vary by the cancer’s type, stage, and spread, as well as a patient’s overall health. Determining the right treatment plan can be complicated, so patients should be sure to discuss it with their medical team, and feel free to ask questions. Learn more about treating endometrial cancer.
Cancer returning after successful treatment is called a recurrence. Even after being declared NED (no evidence of disease), many patients still feel nervous about the cancer coming back. If a patient does experience a recurrence, it will often be within a few years of completing their treatment. The most common site of endometrial cancer recurrence is at the top of the vagina – where the uterus was previously. Fortunately, this site can be evaluated during a speculum exam. Because of this, patients should ensure they have regular appointments with their doctor for follow-up care, and immediately contact their medical team if they experience vaginal bleeding or other symptoms of a possible recurrence.
Treatment for patients with recurrent endometrial cancer will depend on whether the cancer is localized or has spread, as well as the patient’s initial treatment.
The overall 5-year relative survival rate for endometrial cancer is 81%. Survival rates vary depending on how far the cancer has spread when it is initially detected and treated. The 5-year relative survival rate for endometrial cancer that is localized to the uterus is 95%. The 5-year relative survival rate for endometrial cancer that has regional spread to nearby structures or lymph nodes is 70%. The 5-year relative survival rate for endometrial cancer that has spread to distant parts of the body is 18%.
The American Cancer Society estimates that in 2024 about 67,880 new cases of cancer of the body of the uterus will be diagnosed, and about 13,250 women will die from cancers of the uterine body. These estimates include both endometrial cancers and uterine sarcomas.
Up to 10% of uterine cancers are sarcomas, so the actual numbers for endometrial cancer cases and deaths are slightly lower than these estimates. For detailed information about endometrial cancer, visit the American Cancer Society.
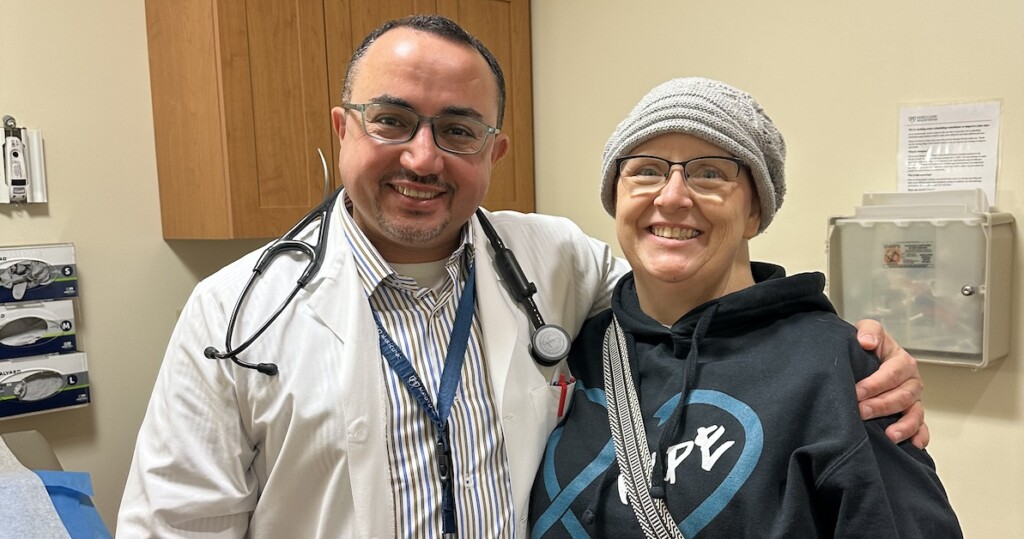
OCRA has several support programs available for those with endometrial cancer, as well as their loved ones. OCRA’s Woman to Woman Peer Mentor Program matches trained survivor Mentors with gynecologic cancer patients. Woman to Woman is offered at sites across the country and is also available through our virtual national mentoring program. Request a peer Mentor through OCRA’s Woman to Woman Peer Mentor Program.
Those with endometrial cancer and all gynecologic cancers are also invited to take part in OCRA’s comprehensive virtual Staying Connected Support Series. Sessions are offered weekly and monthly and cover a variety of topics. Registration is required. View the support series schedule and register today.
OCRA’s online support forum through Inspire offers a place for patients, survivors, and loved ones to connect with others about life with endometrial cancer.
Recognizing the interconnectedness of ovarian and all gynecologic cancers, OCRA expanded its scope in order to accelerate research and broaden our impact on patients’ lives.

Learn about the factors that contribute to ovarian cancer risk and explore prevention strategies to reduce your risk.
Locate gynecologic oncologists, specialists, and treatment centers in your area.
Get email updates about research news, action alerts, and ways to join the fight.