Find a Doctor
Locate gynecologic oncologists, specialists, and treatment centers in your area.
Essential Information for Gynecologic Cancer Patients

After dealing with the initial shock of receiving a diagnosis of ovarian or gynecologic cancer, your next goal will likely be how to go about getting the best care. This page aims to guide you through the treatment process, introduce you to the types of healthcare professionals who will be part of your care team, and provide practical resources to help you make informed decisions. Understanding who will be involved in your care and what to expect can empower you as you navigate new details, learn unfamiliar new medical language, and make key decisions.
Importance of Specialized Care
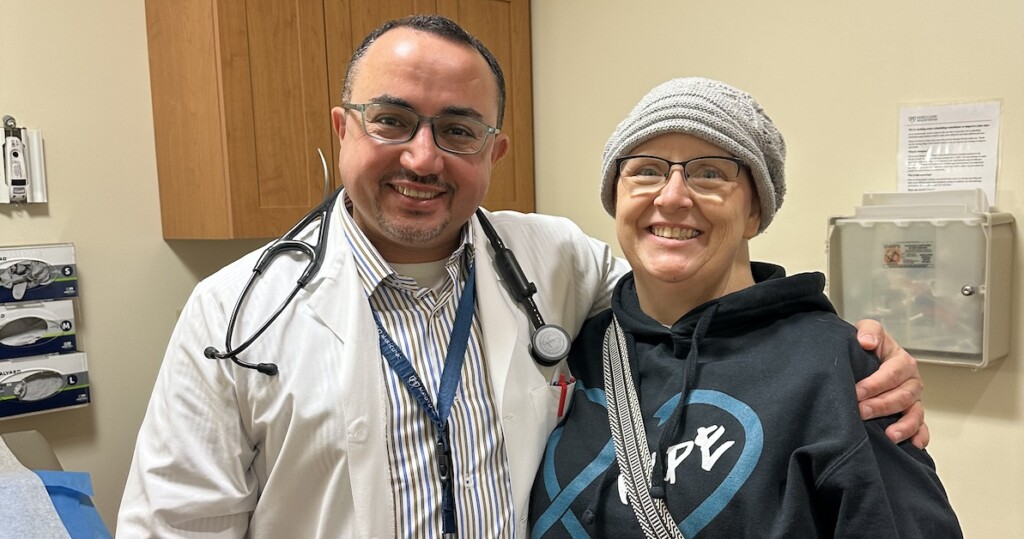
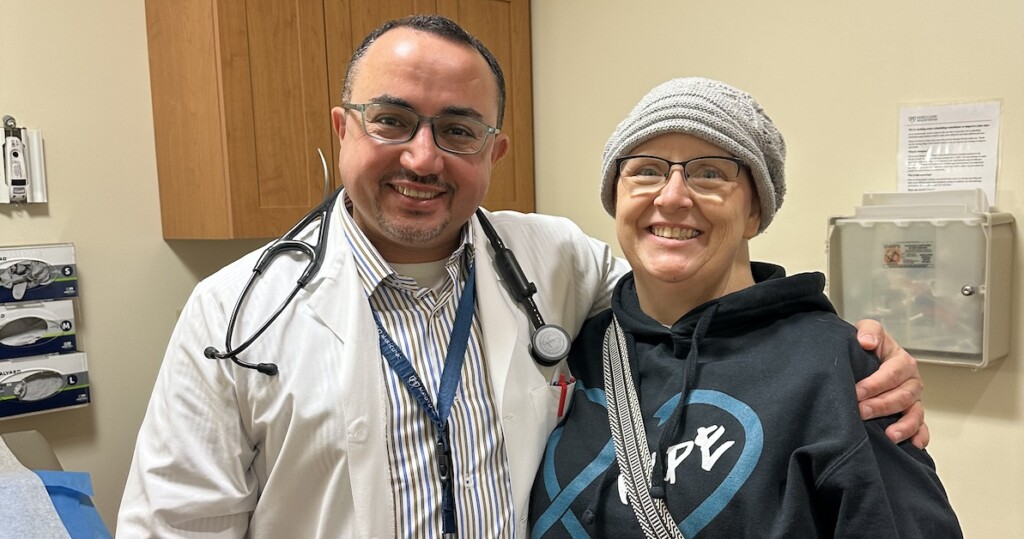
It is crucial to see a gynecologic oncologist as soon as any gynecologic cancer, is suspected. These specialists are trained specifically in the treatment of reproductive tract cancers and significantly improve patient outcomes.
Important Statistics:
Finding a Gynecologic Oncologist
Locate the right specialist for your needs:
Don’t hesitate to seek a second opinion. Most doctors understand your need to explore all options. Consult a gynecologic oncologist experienced with your specific cancer type, and check with your insurance provider about coverage for second opinions.
Understanding The Roles Played in Your Care Team
A comprehensive oncology care team ensures you receive the best possible care; here’s who may be involved in your treatment journey.
Getting Ready for Your First Appointment
Your first appointment with a gynecologic oncologist is important as it will help map out your treatment journey. Here’s how to prepare for it:
Having a clear understanding of your diagnosis and treatment options is crucial. Below are key questions you may want to discuss with your healthcare team. Click on each section to see the questions.
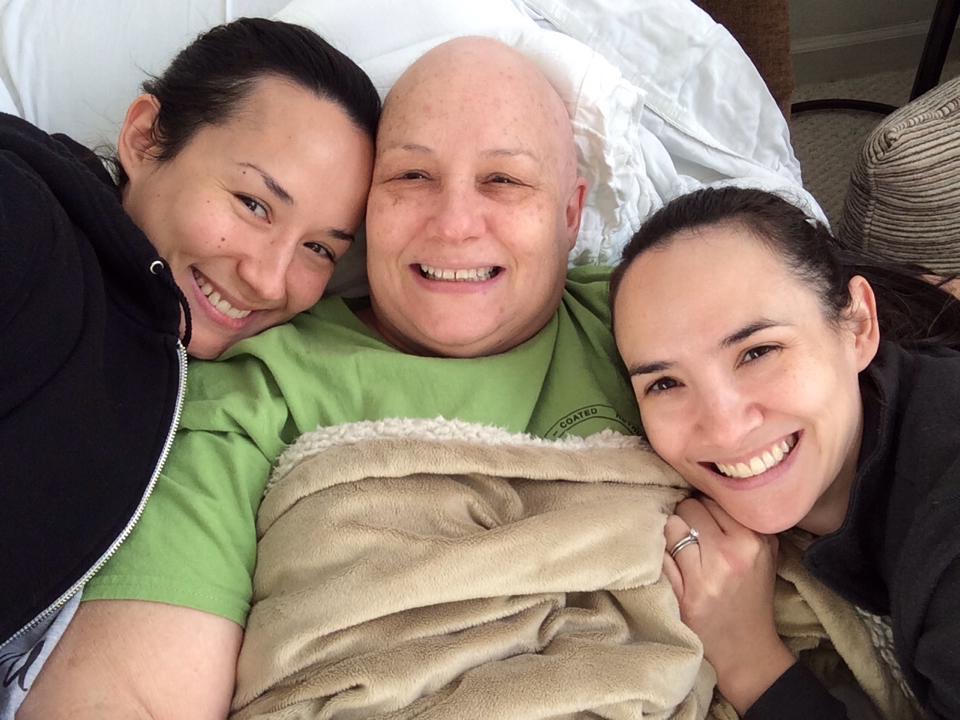
While the primary goals of cancer treatment focus on removing or controlling the cancer, it’s equally important to think about your overall quality of life and future aspirations. Setting personal goals can help align your treatment with what matters most to you.
SMART Goals for Cancer Care
Using the SMART framework can help create and measure meaningful goals:
Questions to Consider
Not all goals will be specific or measurable, but asking yourself the following questions can help you identify how you want to move forward.
Navigating treatment can be challenging, but there are many resources available to support you:
Locate gynecologic oncologists, specialists, and treatment centers in your area.

Explore new treatments for ovarian and gynecologic cancers.
Experiencing side effects from gynecologic cancer treatment is common.
Get email updates about research news, action alerts, and ways to join the fight.