Gynecologic Cancers
Recognizing the interconnectedness of ovarian and all gynecologic cancers, OCRA expanded its scope in order to accelerate research and broaden our impact on patients’ lives.
Vaginal cancer is a rare gynecologic cancer, affecting fewer than 1 in 100,000 women.
Medically reviewed by: Sarah Adams, MD, OCRA Scientific Advisor – August 2025
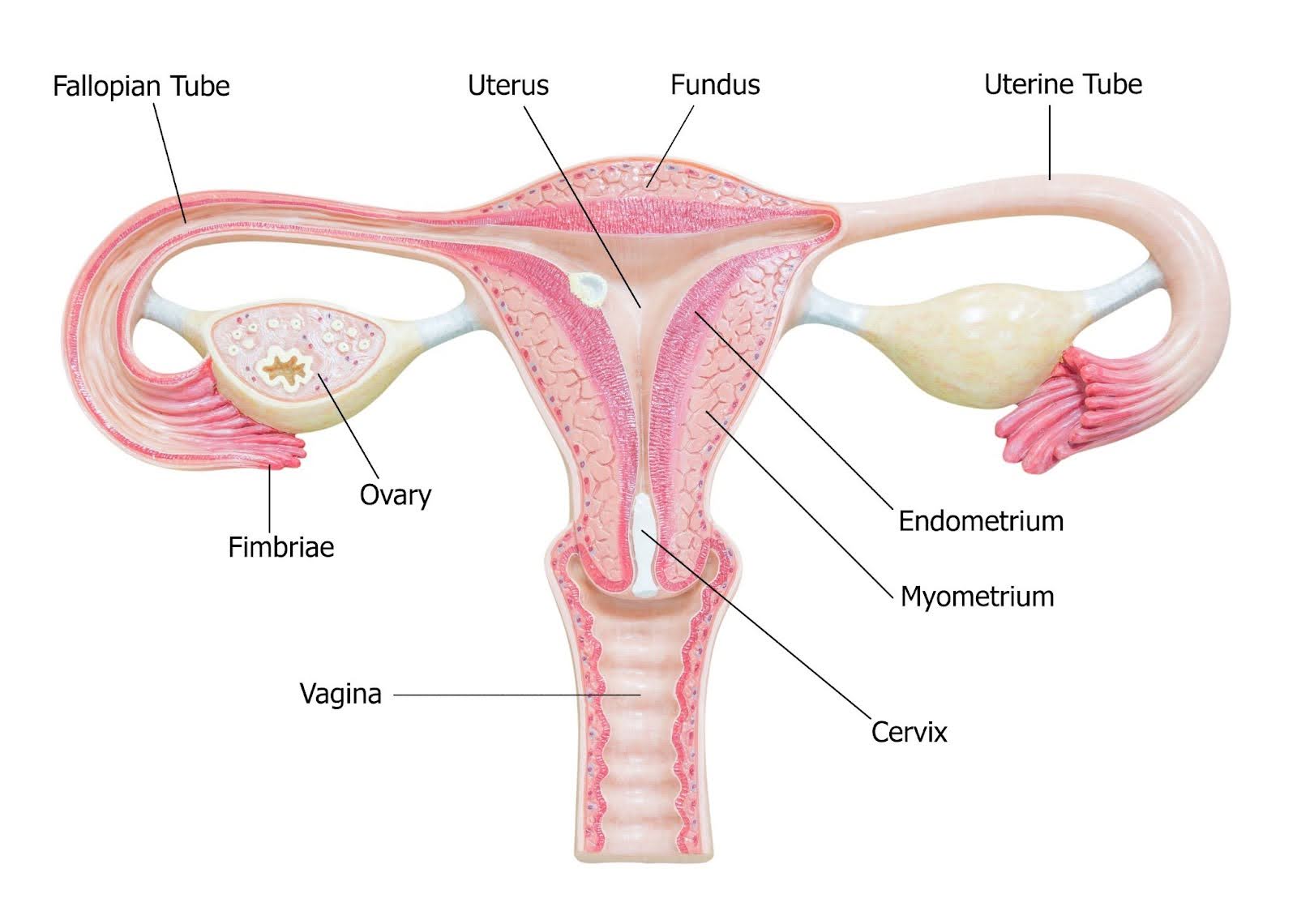
Vaginal cancer starts in the vagina, the tube that goes from the cervix (the lower part of the uterus) to open up at the vulva (the external genitals). About 85% of cases of vaginal cancer are squamous cell carcinomas, which begin in the epithelial lining of the vagina.
Vaginal cancer is a type of cancer that begins in the cells lining the vagina. It differs from cancers that spread to the vagina from other organs, such as the cervix or uterus. Primary vaginal cancer is uncommon and most often affects older women. Early detection increases the chance of successful treatment.
Vaginal cancer may be asymptomatic or may be associated with symptoms depending on the size of the tumor and its location. When present, symptoms of vaginal cancer can include one or more of the following:
Advanced vaginal cancer means the cancer has spread beyond the vagina into nearby parts of the body or lymph nodes. Advanced vaginal cancer symptoms can include painful urination, constipation, pain in pelvis or lower belly, back pain, or swelling in the legs. For more detailed information about vaginal cancer, visit the American Cancer Society.
If you experience any of the above symptoms or have concerns about changes in your vaginal health, consult with a gynecologist or healthcare provider. Early evaluation and diagnosis are important for appropriate care and peace of mind.
Vaginal cancer develops when cells in the vaginal lining undergo changes (mutations) in their DNA. These mutations disrupt normal cell growth, causing cells to multiply uncontrollably and, in some cases, form tumors that can invade nearby tissues or spread to other parts of the body. Approximately 75% of vaginal cancers are caused by HPV (human papillomavirus), according to the American Cancer Society.
Though many who develop vaginal cancer have no clear risk factors, certain factors may increase the chances of developing vaginal cancer, including:
There are several different types of vaginal cancer, including:
A typically slow-developing cancer that starts in the squamous cells of the vagina’s epithelial lining, most commonly in the upper part of the vagina near the cervix. This accounts for approximately nine out of 10 vaginal cancer diagnoses.
A cancer that starts in glandular cells and may be associated with a patient’s exposure to diethylstilbestrol (DES) in utero.
Considered to be a type of mucosal melanoma, an aggressive and extremely rare type of vaginal cancer, usually affecting the lower or outer part of the vagina. This accounts for fewer than three out of 100 vaginal cancer cases.
Sarcomas are cancers that develop in the muscles or connective tissue deep in the wall of the vagina. These are very rare.
There is no dedicated screening tool for vaginal cancer. In some cases, pre-cancerous changes in the vagina can be found with a Pap test — however, these tests are not validated screening tools for vaginal cancer. Vaginal cancers can also be identified during pelvic exams.
A biopsy is ultimately needed in order to confirm a vaginal cancer diagnosis. If a doctor suspects a patient may have vaginal cancer, they may perform tests including:
A doctor will perform a pelvic exam and possibly a Pap test, and will discuss complete medical history, risk factors, and symptoms.
Involves a doctor using a speculum to hold open the vaginal walls to examine the cervix and/or vagina with a colposcope. A colposcope is a magnifying tool to view potentially abnormal areas. Applying vinegar to the walls of the vagina or the cervix during a colposcopy exam can also help identify abnormal cells.
A biopsy is the removal of tissue for further examination, and may be performed if a colposcopy shows an abnormal area suggesting presence of cancer or precancerous changes. The biopsy may be a bit painful, and can produce some cramping after the procedure. This will definitively tell if pre-cancerous or cancer cells are present.
Tests such as a chest x-ray, computed tomography (CT) scan, magnetic resonance imaging (MRI), and positron emission tomography (PET) scan, may be performed after diagnosis of vaginal cancer to determine if and how far the cancer has spread.
Endoscopic tests are not typically used for vaginal cancer, but in some cases a doctor may perform a proctosigmoidoscopy, which is an examination of the rectum and colon with a lighted tube; or a cystoscopy, which checks for spread to the bladder by inserting a thin tube with a lens into the bladder, through the urethra.
See details about vaginal cancer stages from the American Cancer Society.
Depending on the stage of vaginal cancer, or in some cases pre-cancer, doctors will recommend a course of treatment. Treatments for vaginal cancer may include:

OCRA’s online Clinical Trial Navigator is an easy-to-use tool that helps you find clinical trials near you for vaginal cancer. Search by cancer type, treatment history, location, and more.
If cancer returns after treatment, it is called a recurrence. Not every patient will experience a recurrence, but if they do, the cancer may return near the area where it first developed, or elsewhere in the body. Plans for treatment and care should be discussed with a patient’s medical team. Some patients may wish to participate in a cancer clinical trial.
Survivors of vaginal cancer have an increased risk of developing other HPV-related cancers, including vulvar or cervical cancer. Vaginal cancer survivors may also be more likely to develop lung cancer or bladder cancer, though this may be due to the fact that smoking is a shared risk factor for vaginal, lung, and bladder cancer.
Vaginal cancer survival rates vary based on whether the cancer is first detected and treated while it is still localized and how far it has spread. The relative five-year survival rate is 76% for vaginal cancer found at a localized stage. The relative five-year survival rate is 59% for vaginal cancer with regional spread, through the vaginal wall or nearby lymph nodes. The five-year relative survival rate is 24% for vaginal cancer that has spread to distant organs, such as to the liver, lungs, or bones.
The average age of diagnosis of vaginal cancer is 69. According to the CDC, in the U.S., 1,394 women were diagnosed with vaginal cancer in 2022 (the latest year for which data is available) and 438 women died from vaginal cancer in 2022.
There is no guaranteed way to prevent vaginal cancer, but certain proactive steps may reduce the risk:
Talking with your healthcare provider and staying consistent with pelvic exams can help you stay informed and proactive about your health.
OCRA offers several support programs for those diagnosed with vaginal cancer and their loved ones. Through the Woman to Woman Peer Mentor Program, patients are matched with trained survivor Mentors who offer one-on-one emotional support. This program is available at partner sites nationwide and also through OCRA’s national virtual mentoring program. You can request a peer Mentor through the Woman to Woman Peer Mentor Program.
Those with vaginal cancer are also encouraged to participate in OCRA’s comprehensive virtual Staying Connected Support Series. Sessions take place weekly or monthly and explore a variety of topics. Registration is required. View the schedule and register online.
Recognizing the interconnectedness of ovarian and all gynecologic cancers, OCRA expanded its scope in order to accelerate research and broaden our impact on patients’ lives.

Explore new treatments for ovarian and gynecologic cancers.
Locate gynecologic oncologists, specialists, and treatment centers in your area.
Get email updates about research news, action alerts, and ways to join the fight.