BRCA mutations in ovarian cancer are a double-edged sword. While BRCA gene mutation carriers have a significantly higher risk of developing ovarian cancer, BRCA gene mutation in tumors is associated with a significant increase in patient survival. Scientists believe that this is because loss of BRCA gene expression leads to an increase tumor cell response to chemotherapy. Thus, a drug which could turn off BRCA gene expression in BRCA wild-type (non-mutation carrier) tumors, could increase tumor cell response to therapy and thereby significantly increase the survival of these patients. In addition, as loss of BRCA gene expression is associated with response to a new class of drugs known as PARP inhibitors, a pharmacological means to turn-off BRCA gene expression would promote response to PARP inhibitors BRCA non-mutant tumors. Thus a drug which could turn-off BRCA gene mutations in ovarian cancer patients could have a great impact on patient outcomes
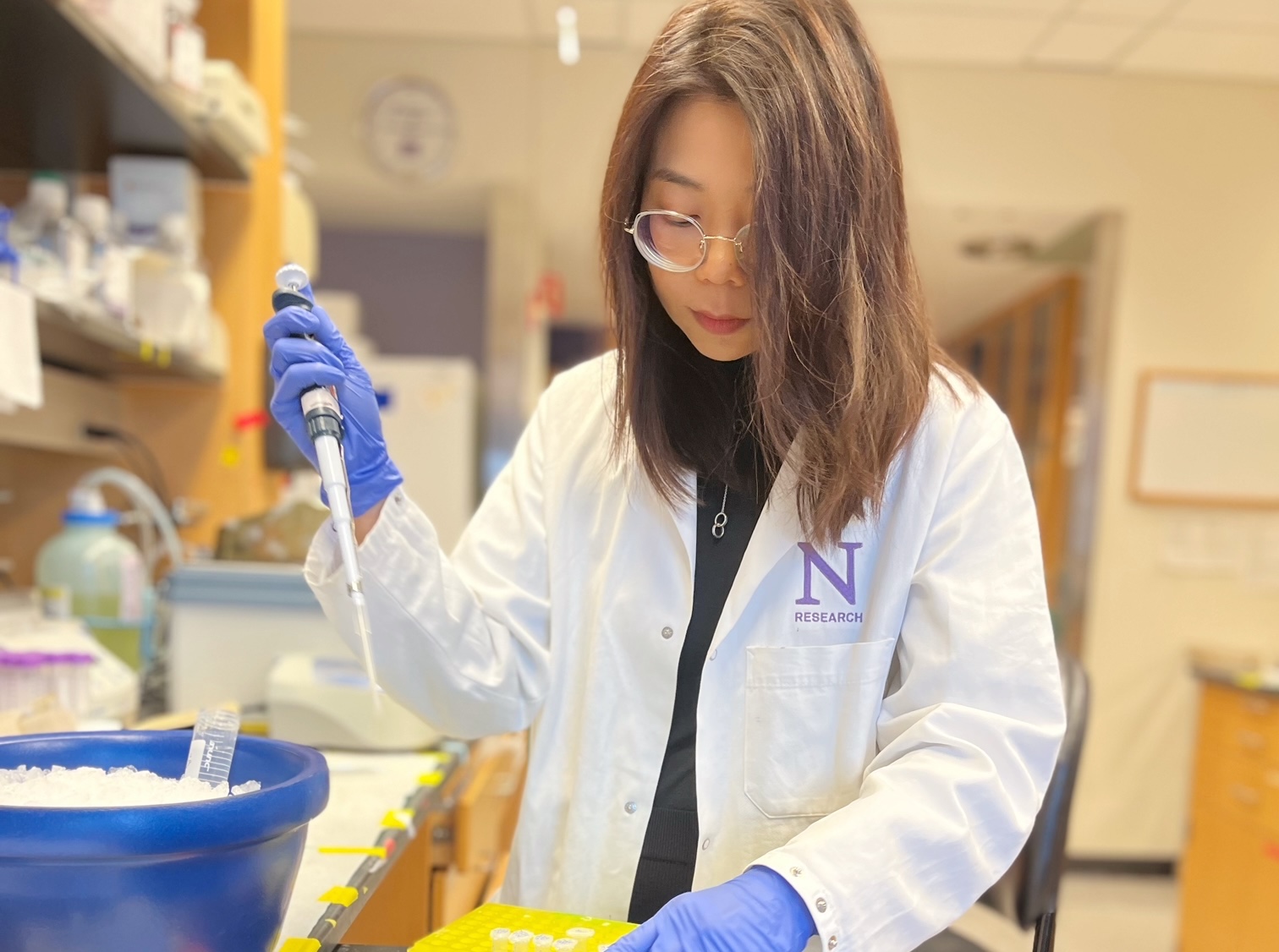
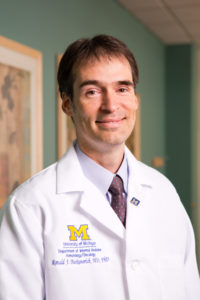
A recent manuscript by Lim and colleagues, including senior author (and OCRF Scientific Advisory Committee) member Ron Buckanovich, MD, PhD and OCRF grantee Ruprecht Wiedemeyer, PhD, now reports the identification of a means to turn off BRCA gene expression in ovarian tumors. They found that the vascular endothelial growth factor receptor-3 (VEGFR3), normally expressed on lymphatic vessels, is also expressed on ovarian cancer cells. More importantly they found that a drug which inhibits VEGFR3, could decrease the levels of both BRCA1 and BRCA2 gene expression. Loss of BRCA gene expression prevented the growth of ovarian tumor cells. Interestingly, ovarian cancer stem-like cells, a population of cells believed to be the cause of disease recurrence, were preferentially susceptible to VEGFR3-mediated growth inhibition. Most importantly drug mediated inhibition of VEGFR3 and loss of BRCA gene expression reversed ovarian tumor chemotherapy resistance and dramatically reduced tumor growth in these preclinical studies. The study predicted that the combination of a VEGFR3 inhibitor and either chemotherapy or a PARP inhibitor would significantly benefit non-BRCA mutation carrier patients with ovarian cancer.
Now, a phase 2 clinical trial by OCRF grantee Joyce Liu, MD and colleagues supports a critical role for targeting VEGFR3 in ovarian cancer. The study treated patients with platinum sensitive recurrent ovarian cancer with the PARP inhibitor Olaparib or the combination of Olaparib and the VEGFR1/VEGFR2/VEGFR3 inhibitor Cedirinib. Patients taking the combination of Olaparib and Cedirinib had a nearly 18 month progression free survival (PFS) period, compared to nine months for patients taking Olaparib alone. Consistent with the study by Lim and colleagues suggesting VEGFR3 inhibition may turn off BRCA gene express, non-BRCA mutation carriers had the most dramatic benefit from combined therapy; BRCA mutation carriers demonstrated an average 16.5 month PFS on olaparib alone and 19.5 month PFS on combination therapy. In contrast, BRCA wild type (or status unknown) patients had an only a 5.7 month PFS on Olaparib alone compared to a 16.5 month PFS on combination therapy.
These studies represent a critical breakthrough for the treatment of patients with ovarian cancer. Phase 3 clinical trials studying the combination of these drugs are currently being planned. Additional studies are being planned to directly determine if Cedirinib is having its primary effect via down regulation of BRCA gene mutations.