
Currently in Treatment
Treatment can bring up lots of questions and concerns. We have answers and up-to-date information.
Experiencing side effects from gynecologic cancer treatment is common. Discover practical tips for managing the side effects of chemotherapy.
Chemotherapy often causes various side effects that can impact your quality of life. Understanding and managing these effects is crucial for navigating life during treatment.
Certain chemotherapy drugs can cause peripheral neuropathy, leading to numbness, tingling, or loss of control in hands and feet. Treatments like acupuncture, massage, and physical therapy can help. Medications such as vitamin B or alpha lipoic acid may also be beneficial. Some patients use ice mittens and booties during taxane therapies to reduce the risk of developing neuropathy. Consult your doctor for the best prevention and management strategies tailored to your individual treatment plan.
Fatigue
Chemotherapy can cause fatigue for many reasons, including by lowering red blood cell levels. Manage your energy by balancing activities you enjoy with scheduled periods of rest. Gentle exercise like walking or yoga can help, but consult your doctor first. Eating nutritious food is also crucial. Your doctor may adjust your chemotherapy dose or prescribe medications if your blood counts are too low.
Insomnia
Chemotherapy and related stress can lead to insomnia. Taking steroids earlier in the day and using cognitive behavioral therapy may help. Always discuss any supplements with your medical team. Dana-Farber Cancer Institute provides more insomnia management tips.
Hair loss is a common side effect of cancer treatment. While your hair will eventually grow back, you might notice a slight change in color and texture. If you are experiencing hair loss, you may choose to wear a wig or you may even decide to cut your hair yourself before beginning to lose it. There are many organizations such as HairWeShare and Locks of Love that provide wigs for those suffering from medically-related hair loss.
Forgetfulness and concentration problems are common after chemotherapy but fortunately for most patients are often temporary (about 15% of patients may experience permanent issues). Though no specific treatment exists, the following tips can help:
For more detailed information, watch this video and visit the National Cancer Institute’s resources on managing chemotherapy side effects.
Poor Appetite
Chemotherapy can change your sense of taste, making food taste salty, bitter, or metallic. Fortunately, this usually normalizes post-treatment. In the meantime, use plastic utensils and a gentle non-alcoholic mouthwash to help reduce the metallic taste. Eat nutritious foods and smaller meals. Consult a nutritionist if needed who can help guide you toward recommended foods (and foods to avoid).
Nausea and Vomiting
Nausea can occur before or after chemotherapy. Anti-anxiety drugs, meditation, and ginger can help. Use anti-emetics for post-treatment nausea. Eat and drink slowly, and stay hydrated.
Diarrhea
Chemotherapy can cause diarrhea soon after treatment. Stay hydrated to prevent dehydration. In severe cases, your doctor may recommend medications to help.
Constipation
Stay hydrated and exercise to address issues with constipation. Consult with your doctor about high-fiber foods, using laxatives, and other options.
Chemotherapy often reduces interest in sexual intimacy due to stress and side effects. A cancer diagnosis can alter your body image and relationships. Rebuilding trust in your body, regaining a positive self-image, and reconnecting with your sexual self can be challenging but is important for overall well-being. For more tips on intimacy, visit Dating, Sexual Health and Intimacy.
Removal of both ovaries leads to surgical menopause in women who were not menopausal before surgery, with symptoms such as hot flashes, night sweats, vaginal dryness, bone density loss, libido changes, and increased cardiovascular risk. For relief, doctors may recommend hormone therapy, vaginal estrogen, or other medications. Discuss lifestyle changes, dietary adjustments, and alternative remedies with your doctor to help manage these symptoms.
Managing Mouth and Lip Sores
Use a soft toothbrush and keep your mouth moist by drinking plenty of fluids. Avoid spicy and harsh foods to prevent irritation.
Infection
Chemotherapy can reduce white blood cell counts, increasing infection risk. To prevent infections, avoid cuts, wash hands often, avoid crowds or visitors that are feeling unwell, stay hydrated, and moisturize dry skin.
Menopause and cancer treatments can cause excessive sweating, including hot flashes and night sweats. Symptoms may include hot feelings, dampness, intense sweating, chills, or drenching sweats. Track your occurrences of sweating in a notebook and discuss possible medications or options for managing it with your doctor.
A cancer diagnosis introduces psychological, emotional, and physical pressures that can increase stress. Elevated stress impacts the body by raising your blood pressure, heart rate, and blood sugar. Consider utilizing stress management methods such as counseling, talk therapy, social support, exercise routines, or medication.
Feelings of sadness and grief are common during cancer treatment. Depression can result from the diagnosis itself, hormonal changes, and/or treatment side effects. The stress of dealing with everything can often feel overwhelming.
The American Cancer Society estimates that 1 in 4 cancer patients may experience clinical depression. If you are experiencing severe and lasting symptoms, contact your doctor or seek medical help. If you are experiencing thoughts of self-harm, call or text the National Suicide Prevention Lifeline at 988.
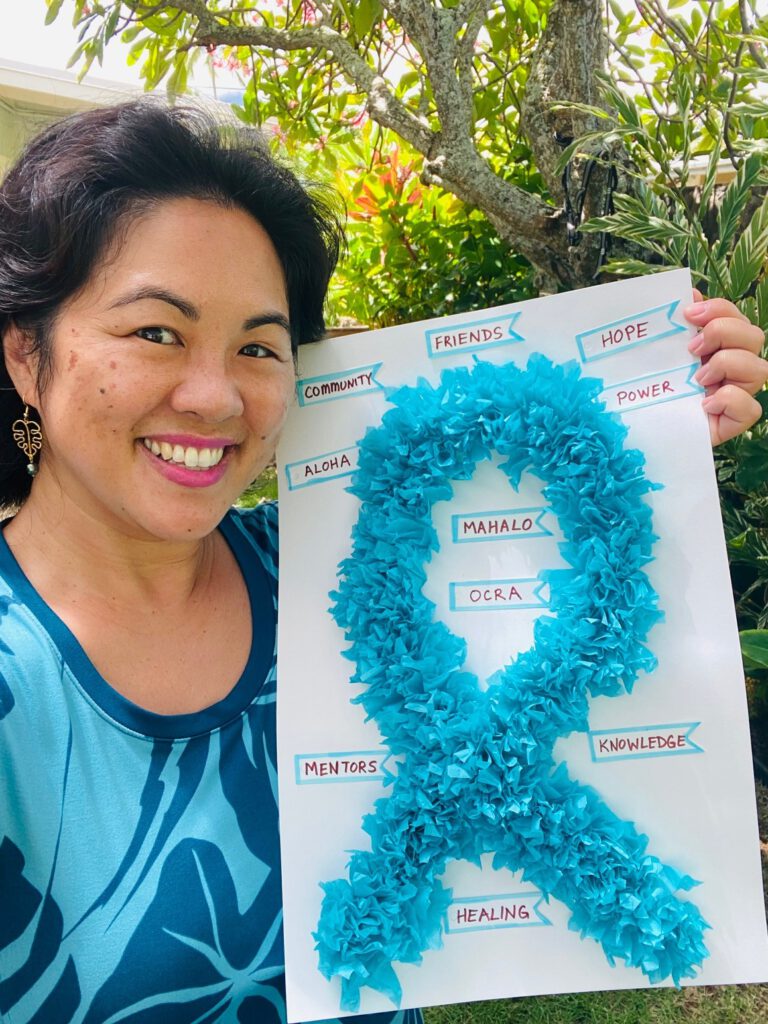
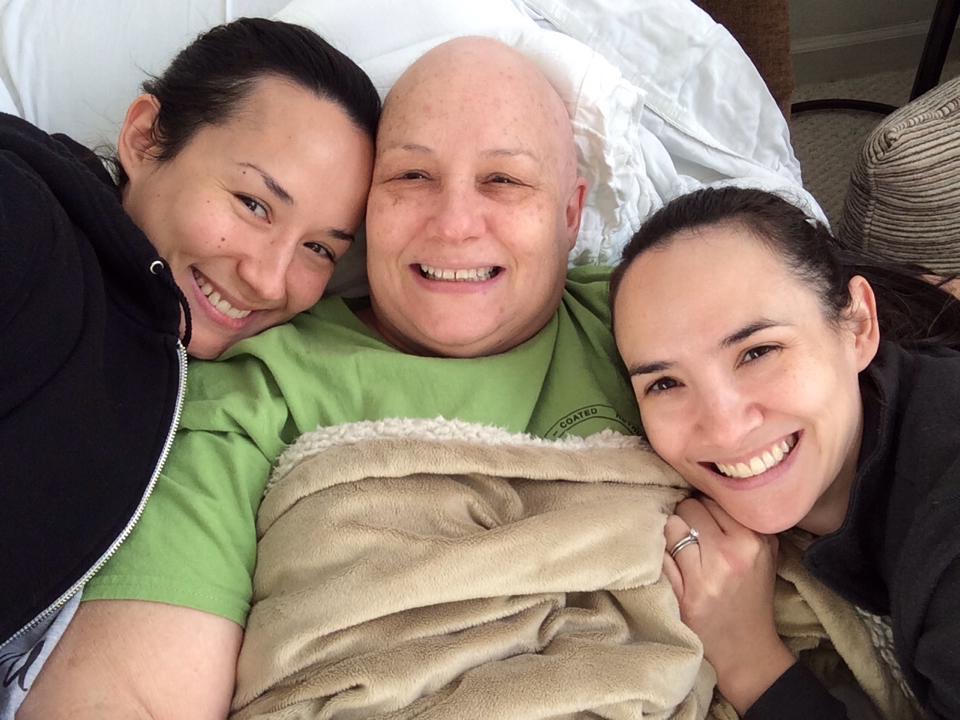
OCRA’s virtual support series welcomes gynecologic cancer patients and survivors, as well as loved ones, to meet online to talk about things like a new diagnosis, recurrence, relationships, and more. Connect with people who understand exactly what you are going through. Find a session today. Registration is required.
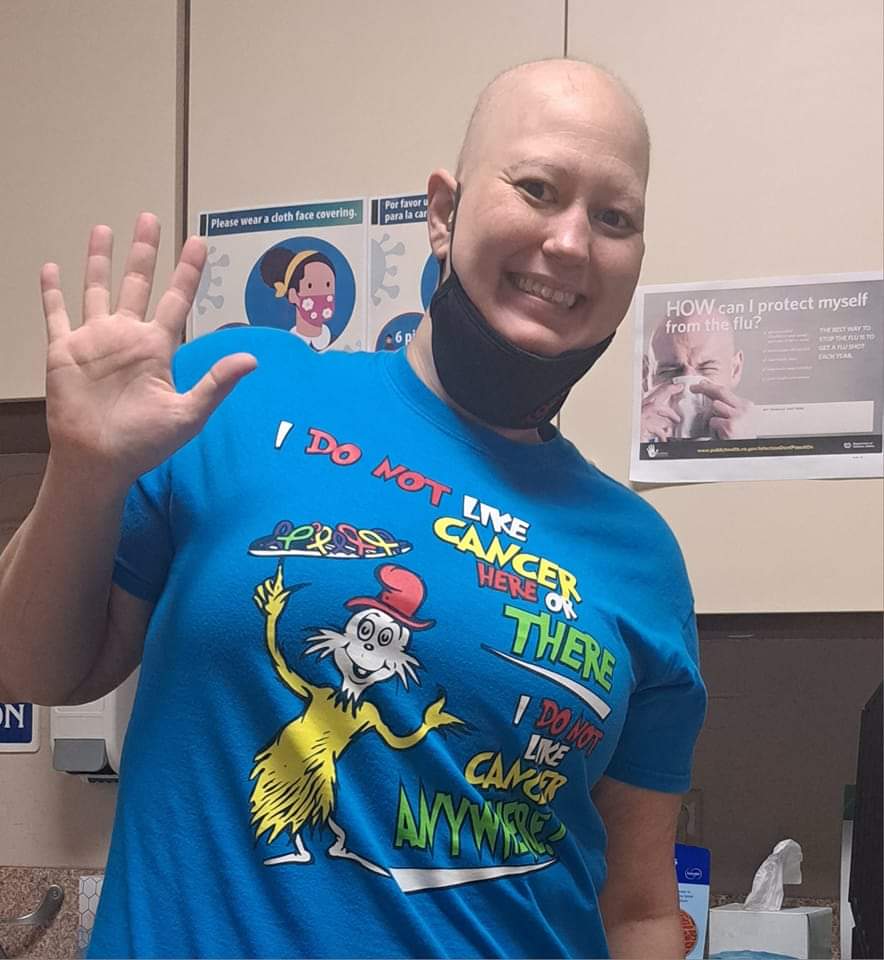
My cancer care team has loved me like family and cheered me on since chemo #1. I completed chemo in September. And wanted to ring that bell for everyone fighting out there!

Treatment can bring up lots of questions and concerns. We have answers and up-to-date information.

Find a trained survivor Mentor to offer one-on-one emotional support and guidance.

Many patients find substantial relief through integrative therapies, dietary changes, palliative care, and more.
Get email updates about research news, action alerts, and ways to join the fight.