Find a Doctor
Locate gynecologic oncologists, specialists, and treatment centers in your area.
CA-125 is a biomarker for ovarian cancer that is often elevated in the blood of people with ovarian cancer. It is important to understand that while the CA-125 blood test is useful when diagnosing and monitoring people with ovarian cancer, a CA-125 test alone is not an accurate diagnostic tool. In fact, no single test currently exists that can accurately detect ovarian cancer in its earliest stages. This is a gap that researchers, including those with projects funded by Ovarian Cancer Research Alliance (OCRA), are actively working to close.
Medically reviewed by: Sarah Adams, MD, OCRA Scientific Advisor

CA-125 stands for Cancer Antigen 125, a protein released into the bloodstream and found at higher levels in many, but not all, ovarian cancer cases.
Because of this variability and the fact that CA-125 can also rise due to non-cancerous conditions, the test is not used alone for diagnosis. It’s typically ordered when symptoms or imaging suggest concern, but not for routine screening in the general population.
An elevated CA-125 level, commonly defined as above 35 units/mL does not automatically mean someone has cancer. Many benign or unrelated conditions can also raise CA-125 levels.
This is why CA-125 is usually interpreted alongside other tests, such as imaging or pelvic exams, and in the context of a person’s symptoms, age, and menopausal status.
While it’s not recommended for routine screening, the CA-125 test does play a role in ovarian cancer care:
However, while CA-125 can detect recurrence before symptoms appear, studies have shown that starting treatment earlier based solely on rising CA-125 levels does not improve overall survival or quality of life. As a result, some guidelines recommend individualizing its use in post-treatment monitoring, based on patient and physician decision-making.
If CA-125 is linked to ovarian cancer, why isn’t it used to screen all women annually? The answer lies in its limitations:
False positives can occur due to benign conditions (like fibroids, endometriosis, or even pregnancy).
Because of this, organizations like the National Cancer Institute and the U.S. Preventive Services Task Force do not recommend CA-125 for screening average-risk women.
Unfortunately, no. As of now, there is no proven method to screen for ovarian cancer that reduces mortality. That includes transvaginal ultrasound, CA-125, or using both together. Studies show that even with these tools, women in screening groups were:
According to a summary published in American Family Physician, both the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) and Prostate, Lung, Colorectal, and Ovarian (PLCO) trials failed to demonstrate a survival benefit from screening, and highlighted the harms of unnecessary surgery triggered by false-positive results.
The ROCA (Risk of Ovarian Cancer Algorithm) test estimates current risk by analyzing changes in CA-125 over time, together with age and menopausal status. Large trials show no mortality reduction from ROCA-based screening, so it is not recommended for routine screening. In select higher-risk situations, some clinicians may discuss it to guide follow-up. It can be purchased with a doctor’s order.
If a doctor suspects ovarian cancer typically due to symptoms, imaging, or a high CA-125 level, a surgical procedure is usually needed to confirm it:
In some cases, fluid from the abdomen (ascites) may be sampled for diagnosis, but surgery is generally required for certainty.
The CA-125 test can be helpful, but only in the right context. It’s not a screening tool for the general public, and a high result doesn’t necessarily mean cancer is present. As we continue to push for better early detection methods, OCRA is investing in research that can make that future a reality.
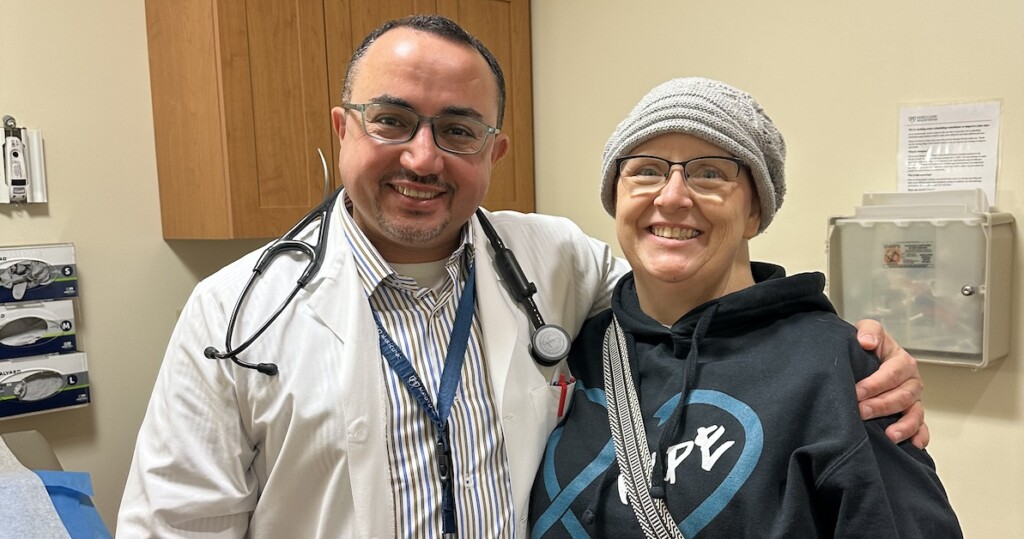
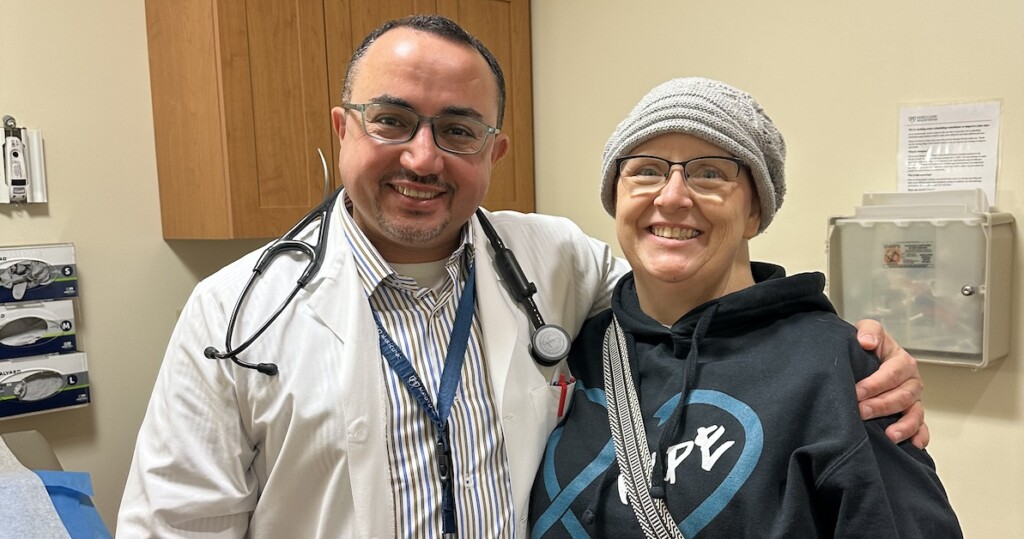
If you’re concerned about ovarian cancer symptoms or risk factors, we encourage you to find a gynecologic oncologist and speak with them about your options.
You may also be eligible for OCRA’s Free Genetic Testing Program, which helps individuals assess hereditary cancer risk through at-home BRCA and related mutation screening, at no cost if you qualify.
Locate gynecologic oncologists, specialists, and treatment centers in your area.

Learn about the factors that contribute to ovarian cancer risk and explore prevention strategies to reduce your risk.
Recognizing the interconnectedness of ovarian and all gynecologic cancers, OCRA expanded its scope in order to accelerate research and broaden our impact on patients’ lives.
Get email updates about research news, action alerts, and ways to join the fight.