
Getting the Best Care
Get guidance on treatment and access resources to make informed decisions.
Every day, 54 people in the U.S. are diagnosed with ovarian cancer. Learn about the disease, from causes and risk factors to the many subtypes and more.
Ovarian cancer occurs when cells in the ovaries begin to grow uncontrollably and invade nearby tissues. There are several types of ovarian cancer, each originating from different cell types within the ovary.
Ovarian cancer is classified based on the type of cells where it originates. Below, you can learn more about each type. Click on each section to expand for more details.
Epithelial ovarian cancers are the most common type, originating from the surface cells of the ovary. They include several subtypes, click on each subtype for more information.
The most common subtype, making up about 75% of epithelial ovarian cancers.
A less aggressive form compared to HGSOC.
A rare subtype that may be associated with endometriosis.
Rare type of epithelial ovarian cancer that is more likely to be diagnosed while it is still confined to the ovaries.
Also known as tumors of low malignant potential (LMP).
Germ cell tumors originate from the reproductive cells (egg cells) of the ovary and are rare. They include:
Malignant tumors with poorly-differentiated cells.
The most common malignant germ cell tumor.
A type of germ cell tumor often diagnosed in children and young adults.
Stromal cell tumors arise from the connective tissue cells of the ovary and are very rare. They include:
The most common type of malignant sex-cord stromal tumors.
Rare tumors that may produce hormones like androgens.
Some rare ovarian cancers may include features of different cell types or have unique characteristics:
Malignant mixed Mullerian tumors containing both epithelial and stromal elements.
Extremely rare, highly malignant tumor.
In many cases, ovarian cancer does not produce noticeable symptoms until the disease is in advanced stages. Symptoms associated with ovarian cancer can sometimes be mistaken for other common problems.
Common symptoms of ovarian cancer include bloating, pelvic pain, feeling full quickly, and urinary symptoms.
While the exact causes of ovarian cancer remain unknown, both acquired and inherited genetic mutations can play a role.
If a doctor suspects ovarian cancer, they may perform tests such as a pelvic exam, ultrasound, CT scan, or CA-125 blood test to learn more. Surgery is the only way to make a definitive diagnosis of ovarian cancer.
If you or someone you love is diagnosed with ovarian cancer, it’s natural to be concerned about survival rate (prognosis), treatment, and whether a cure is possible. Understanding how ovarian cancer is staged and what each stage means can give you an idea of what to expect.
After receiving an ovarian cancer diagnosis, you will meet with your healthcare team to discuss the best treatment options for you. Seeking care from a gynecologic oncologist, a specialist in women’s reproductive cancers, is strongly recommended for better outcomes.
Recurrence of ovarian cancer is when the cancer returns after treatment.
For comprehensive and up-to-date information on ovarian cancer statistics, including prevalence, survival rates, and more, visit our detailed statistics page.

Get guidance on treatment and access resources to make informed decisions.
Recognizing the interconnectedness of ovarian and all gynecologic cancers, OCRA expanded its scope in order to accelerate research and broaden our impact on patients’ lives.
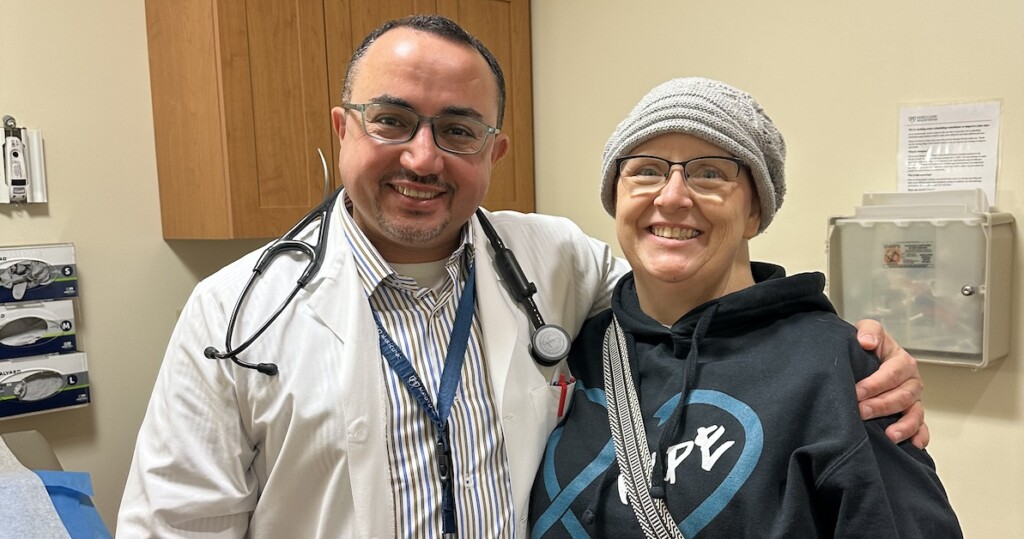
Locate gynecologic oncologists, specialists, and treatment centers in your area.
Get email updates about research news, action alerts, and ways to join the fight.