“It’s kind of like how the Apollo mission to the moon gave us Velcro.”
Dr. David Chapel and his team are laying new groundwork in better understanding the origins of high-grade serous carcinoma, even if the exact applications are hard to see this early on. David, an OCRA grantee, speaks with great passion when he describes his work. As a pathologist, he is focusing not just on the location in the body where the tumor may originate, but he’s seeking a better understanding of what mutations may be taking place on the cellular level.
“You don’t always know what precise developments are going to come out of specific projects,” he said about the nature of scientific research. “But as long as you investigate the fundamental biology of the disease, there will always be innovative minds out there who can synthesize the data and take it in a new direction.”
David is finishing up a fellowship at Brigham Women’s Hospital and will be a Clinical Assistant Professor at the University of Michigan this fall, which is where his study of microbiology began.
An early interest in medical research
Although David grew up on a farm in rural Michigan, a farm that had been in his family for seven generations, he started thinking about a career in medicine back in high school. His father was a pharmacist and his mother worked in a hospital laboratory, and he had spent time growing up in both the pharmacy and the clinical lab.
“I knew in high school that I wanted to go into a career that would involve lifelong learning,” David said, “and something that would involve contributing to our knowledge of human disease.”
Early on in his undergrad career at the University of Michigan, David got very interested in microbiology as he learned about the “stunning” breadth of diversity in bacteria. His interest was honed even further toward cancer and neoplasia (the growth of abnormal tissue) while in medical school at Columbia University.
Speaking about the field of pathology, David acknowledges that it isn’t the most sought after profession in medicine, and believes that this may be due to lack of awareness of the field itself among medical students. But his eyes were opened early on as his mother worked with pathologists in her lab.
“As a pathologist,” David explained, “you’re really behind the scenes supporting clinical care in a way that isn’t as public facing.”
What is gynecologic pathology?
Simply put, pathology is the study of disease. But it is a broad field that can be roughly divided into three main categories: clinical pathology, which pertains to the analysis of bodily fluids (think blood draws, urine tests); anatomic, which is the study of more solid human tissues (like biopsies); and molecular, a newer field that explores DNA sequencing or protein analysis.
David’s work is in anatomic pathology, studying the tissues of the female reproductive tract. He was drawn to gynecologic pathology in large part to the wonderful mentors he had during his residency. He’s also fascinated by the unique qualities of the tissues within the female reproductive tract, which undergo normal cyclical changes.
“There are changes that happen on a monthly basis, which introduces different morphological patterns that we see under the microscope,” he said. “This makes it a very interesting field to study from a microscopic standpoint. There’s something about the temporal and spatial heterogeneity of it.”
Exploring the endometrium
The endometrium is the inner lining of the uterus, which thickens and thins every month according to a woman’s menstrual cycle. Endometriosis is a disease whereby this lining leaves the uterus and does not necessarily go in the right direction. Rather than flow out of the vagina, as would happen during a normal period, this lining might flow back through the fallopian tubes into the peritoneal cavity.
One of the things that David is exploring in his lab is whether the origins of some forms of ovarian cancer could be traced to the endometrium.
“It’s interesting that given how common, relatively speaking, and aggressive high grade serous carcinoma is in the ovary, that we haven’t really understood where it comes from until about 15 years ago,” David noted, referring to the discovery of lesions at the tips of the fallopian tubes that led to the realization that this form of ovarian cancer may arise there, and not in the ovaries as previously had been thought.
This discovery led to a paradigm shift in how this common form of ovarian cancer may be treated, and how risk for the disease could be greatly reduced. And yet, it’s also known that only about half of high grade serous carcinomas are associated with these tubal precursor lesions.
“So that, of course, raises the question: what’s the deal with the other half? Are they arising from tubal precursors that are really subtle so that we can’t see them?” David asks. “Or are they arising from someplace else, perhaps some other potential precursor cell that is not in the fallopian tube?”
This is the main focus of David’s research this year: trying to explore whether endometrial cells may flow backwards through the fallopian tubes, and whether these cells contribute to the origin of high grade serous carcinomas.

Gaining insights, laying groundwork
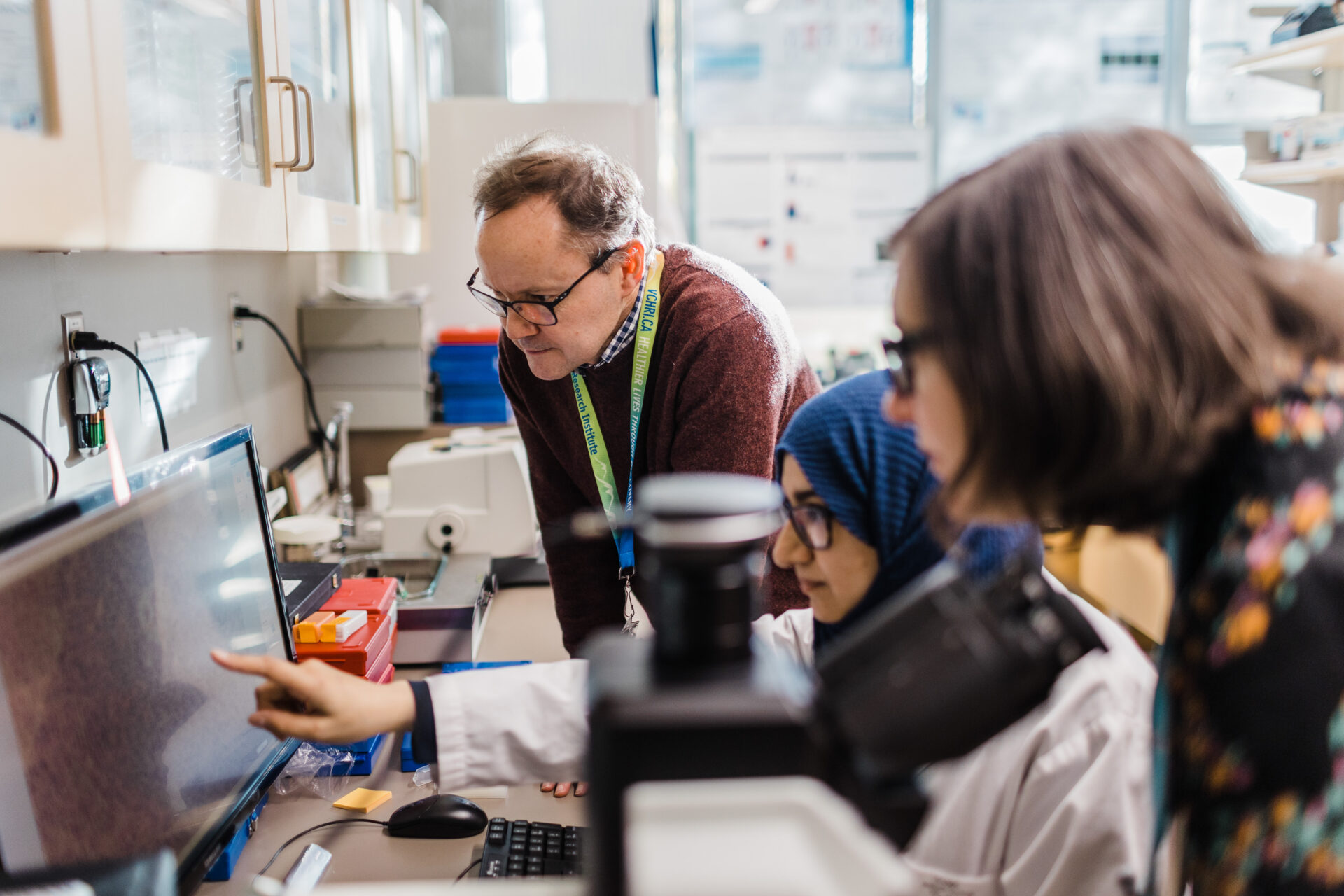
David and his team are looking at hysterectomy specimens from patients diagnosed with high grade serous carcinoma, using a technique called immunohistochemistry to screen for an altered protein in the endometrial lining cells. They are looking for a shared mutation between the tumor itself and the abnormal lesion in the endometrium.
“If you have the same mutation at both sites, it’s very likely that the two lesions are clonally related to each other,” he said. “And that would suggest that in some cases, this early endometrial precursor is giving rise to the cancer that presents itself in the abdominal cavity.”
What this means, is that it’s possible that a screening could one day look for mutated cells in the endometrium.
David is quick to point out that the technology is not there yet. Researchers would not only have to figure out how to detect this mutation, but also determine whether these mutations are simply incidental or actually predictive of cancer. But he believes that this line of research, showing that the endometrium could at least possibly be linked to ovarian cancer, is the first step in developing a screening test.
“I feel like we’re laying the groundwork, though the precise applications are hard to see early on,” he said. “And [the OCRA] grant has been a tremendous source of support and has enabled me to do more dedicated research that otherwise wouldn’t have been possible.”
Dr. Chapel, we are just as grateful to you – and all of our grantees – for the work you’re doing to advance our understandings of this disease. And we are grateful to the following OCRA Community Partners who have helped to fund Dr. Chapel’s work: Janice Lopez Ovarian Cancer Foundation, Teal There’s A Cure, Tell Every Amazing Lady About Ovarian Cancer, and Toasting to Teal.