Palliative care is one of the most misunderstood areas of the medical world, starting from its pronunciation (“PAL-ee-uh-tiv”), all the way to who it can help, and what it entails.
Dr. Beth Popp, of Icahn School of Medicine at Mount Sinai, joined us at this year’s virtual Ovarian Cancer National Conference to answer some frequently asked questions about palliative care, with special attention paid to how it can benefit those managing life with ovarian cancer.
What is Palliative Care?
Palliative care is a medical subspecialty, just like cardiology or gastroenterology. Its focus is on improving quality of life for those managing a serious illness, by addressing the symptoms that can accompany both the disease and its treatment. Palliative care is provided alongside curative treatment, and can be beneficial for patients at any age, and any stage of disease.
When cancer strikes, the goal is to achieve a cure or keep the cancer’s growth in check; to maintain good function and quality of life; to have coordination and connection of care; and to have the support to make informed decisions. Palliative care can help with all of this.
Dr. Beth Popp, Icahn School of Medicine at Mount Sinai
Depending on the medical institution, palliative care can be provided by a team of specialists, or even by an individual oncologist. If you are currently in treatment for ovarian cancer and have not had a conversation with your primary care physician about palliative care, don’t be shy about asking what is available and how it can help you.
Why would someone get palliative care?
First, because it’s an official recommendation from the American Society of Clinical Oncologists (ASCO). Per ASCO’s Clinical Practice Guidelines 2017 Update, “Patients with advanced cancer, whether inpatient or outpatient, should receive dedicated palliative care services, early in the disease course, concurrent with active treatment … Providers may refer caregivers of patients with early or advanced cancer to palliative care services.”
And, to put it simply—it just makes sense. It goes without saying that diagnosis and treatment of serious illness, like ovarian cancer, takes both a physical and emotional toll. Treating the pain, symptoms and stress that often go hand-in-hand with cancer can make a major positive difference in a patient’s everyday life. Early integration of palliative care, along with disease-directed care, can give a patient the tools needed to get back to enjoying life, and can even lead to improved outcomes.
Palliative care can relieve a range of symptoms and stresses for those facing serious illness, including:
- Pain and neuropathy from disease and treatment
- Sleep issues
- Fatigue
- Anxiety, depression and mood fluctuations
- COVID-19 stresses
- Increases and decreases in appetite
- Weight loss and weight gain
- Body image issues
- Intimacy and sexuality challenges
How can palliative care help with ovarian cancer?
Patients undergoing treatment for ovarian cancer face unique challenges that palliative care can help address and alleviate.
- Because of the way ovarian cancer develops and presents, cases are often caught in later stages.
- The symptom burden–the full weight of all symptoms being experienced, which have an impact on quality of life–on ovarian cancer patients is high, from both the cancer itself and the therapies most commonly used to treat it.
- Medical providers are often unaware of the symptom toll on patients, making them less likely to offer options for relief.
- Ovarian cancer as an illness has lots of ups and downs, and can require many decisions surrounding treatment and care.
Interested in learning more about how palliative care can improve quality of life for those managing the unique symptoms and side effects from ovarian cancer? Watch the full presentation, Living with Ovarian Cancer: How Palliative Care Can Help.
A palliative care team or provider can work with patients and families to find the right combination of medicines to control debilitating side effects, match goals to treatment options, address gaps in care that can lead to unnecessary hospital stays, and help everyone involved to adjust to the disease and the changes it brings with it.
Common questions about palliative care:
How do I know if I need palliative care?
Need is based on symptoms, not on disease prognosis. This means that no matter the stage of disease, as long as symptoms are present–physical or otherwise–palliative care can be helpful and worth pursuing. There is also no age requirement; palliative care can be just as restorative for pediatric patients as it is for those who are older.
How is palliative care paid for?
Palliative care is paid for and covered just like any other medical subspecialty. Most insurance, including Medicare and Medicaid, cover these medical services, as do many private insurers. Insurance companies vary in their requirements around referrals and other details, so it’s important to look into your insurance plan before proceeding.
Why is palliative care a separate specialty—can’t my oncologist do this?
Some do! But generally speaking, palliative care addresses needs the U.S. healthcare system has historically not been equipped to resolve. Though things are shifting, U.S. healthcare has sometimes operated as more of a “sick-care” system, focusing on technology and disease-driven care that doesn’t take into account quality of life considerations. Until recently, outside of palliative care, most physicians were not trained to assess or adequately treat the symptoms or stress that can accompany serious illness, and to communicate effectively with patients about these issues.
Should I wait for my doctor to bring up palliative care?
Palliative care must be coordinated through your primary care physician. If you are managing a serious illness and experiencing symptoms or treatment side effects, and have not yet discussed palliative care with your primary medical team, there is no need to wait for your physician to bring it up. Your PCP may not realize you’re experiencing symptoms that need to be addressed. Ask about what is available to you, and advocate for yourself! Explain to them that you would like an extra layer of support, and need a referral. If they are hesitant, you can refer them to GetPalliativeCare.org for more information.
Where can I learn more about palliative care?
For a clear and comprehensive look at palliative care, visit GetPalliativeCare.org. You can take a quiz to learn if palliative care may be right for you, find tips on talking to your doctor, listen to patients’ stories, and search for palliative care providers near you.
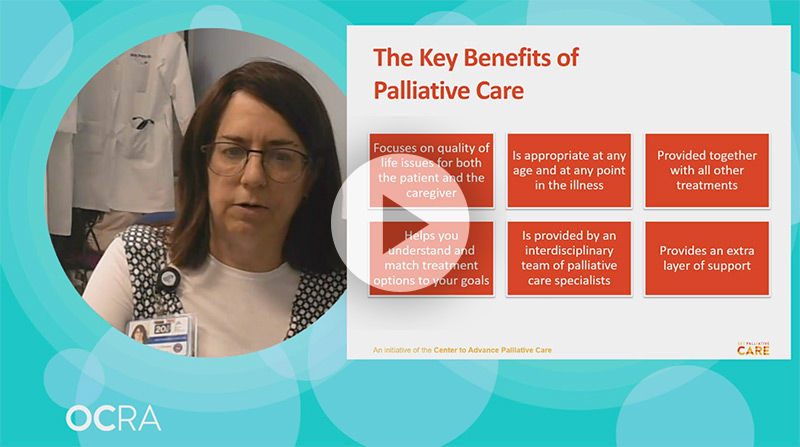
Watch now: “Living With Ovarian Cancer: How Palliative Care Can Help,” and other informational videos originally presented at our 2020 virtual National Conference are now available in their entirety on our website. View all ovarian cancer videos.