The first part of this year’s annual meeting of the AACR was titled “Discovery Science Driving Clinical Breakthroughs” and was held virtually from April 10 to 14, 2021.
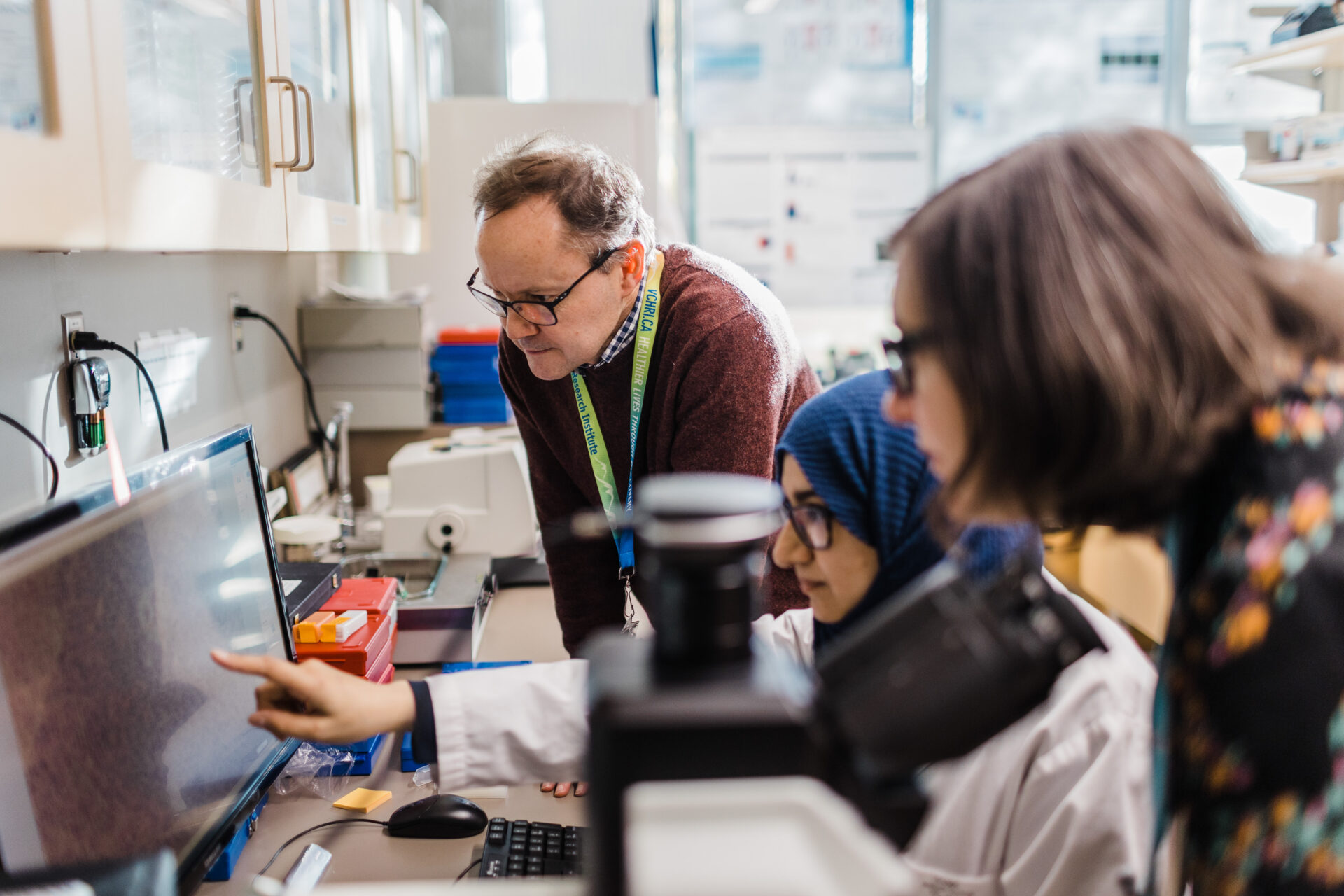
Two OCRA Research Advocates, Elise Daniel and Annie Ellis (a member of OCRA’s Scientific Advisory Committee), participated in the Scientist<->Survivor Program (SSP), which is designed to build enduring partnerships among the leaders of the scientific and patient advocacy communities worldwide. This year’s SSP included small group lectures on Cancer 101, Cancer Genetics, Clinical Trial Development, and Digital Pathology.
Following are highlights of some of the prevailing themes of the 5-day Annual Meeting, compiled by Elise Daniel and Annie Ellis. We’re grateful for their work in presenting these important highlights to the ovarian cancer community.
As most presentations involved preclinical findings that are not yet published or actionable, this report provides only a brief overview of what was discussed.
Ovarian Cancer
Dr. Kunle Odunsi, of the University of Chicago Medicine Comprehensive Cancer Center and member of OCRA’s Scientific Advisory Committee, chaired a session on Targeted Therapy and Ovarian Cancer Clinical Trials which included the results of two Phase I clinical trials for platinum resistant and refractive ovarian cancer which warrant further investigation.
- Dr. Jermaine Coward, of ICON Cancer Centre in South Brisbane, Australia presented “TRX-E-002-1 in treatment-refractory ovarian cancer: Final phase 1 study results from the dose-escalation and dose-expansion cohorts.” This trial was held in Australia and USA and included heavily pretreated patients. TRX-E-002 (Cantrix) is administered intraperitoneally (IP) and some patients received standard chemotherapy after receiving TRX-E-002. Results suggest that TRX-E-002 may sensitize cancer cells to standard chemotherapy.
- Dr. Jeffrey Goh, of ICON Cancer Centre in South Brisbane, Australia presented “Safety/tolerability and preliminary antitumor activity of sitravatinib plus tislelizumab in patients with advanced platinum-resistant ovarian cancer (PROC).” Sitravatinib is an oral targeted therapy and tislelizumab is an anti-PD1 agent. Most of the patients were heavily pretreated patients and best responses were seen in patients who had not been previously exposed to anti-PD-1/PD-L1 agents. Read “islelizumab/Sitravatinib Shows Early Antitumor Activity, Safety in Platinum-Resistant Epithelial Ovarian Cancer” in OncLive.
Ovarian Cancer Poster Sessions
- Siqi Hu, a PhD candidate at the University of Utah Huntsman Cancer Institute, presented a poster titled “Health Disorders among Ovarian Cancer Survivors in a Population-Based Cohort.” This work suggests that women diagnosed with ovarian cancer were more than three times more likely than the general public to be diagnosed with depression and anxiety disorders, especially within the first two years post diagnosis. The study also aimed to look at risk factors for such mental illness among survivors. The study suggests that ovarian cancer patients would benefit from mental health services during their cancer treatments and beyond. Ongoing research could help oncologists and patients better prepare for the possibility of these issues occurring.
- Dr. Jocelyn Chapman of the University of California, San Francisco presented a poster titled “Circulating tumor DNA predicts disease recurrence in ovarian cancer patients.” In this very small study, samples were collected before surgery and collected serially after surgery in some patients. Patient-specific circulating tumor DNA (ctDNA) assays were designed using whole exome sequencing on patient tumors and matched normal tissue. In the patients with serial ctDNA collection for six months after surgery, all with detectable ctDNA (7/7) had relapsed and none without detectable ctDNA (13/13) relapsed within a median 29-month follow up period. The authors observed that presence of ctDNA was a strong predictor of relapse and suggest that monitoring ctDNA could be a useful tool in clinical decision making for patients.
Symptom Science
During a Special Session, Cobi J. Heijnen, from MD Anderson Cancer Center, talked about studies looking at the mechanisms of chemobrain accelerated aging, as well as peripheral neuropathy resulting from chemotherapy. She noted that chemobrain remains an issue for 17-34% of patients after treatment is completed, and that there are no approved preventive or responsive treatments for it. Peripheral neuropathy resulting from chemotherapy remains in 70-75% of patients who experience it. Her study is geared to understand cognitive loss in response to cisplatin therapy to consider cell therapy treatments for both cognitive changes and peripheral neuropathy. Early findings in mouse models suggest that administering mesenchymal stem cells or isolated mitochondria via nasal passages can reverse mitochondrial deficits, brain damage, and cognitive deficits and pain. She also noted that accelerated brain aging in older patients (grey matter atrophy) was analogous to 4 years of aging, resulting in higher DNA damage that negatively impacted attention and motor speed scores.
Artificial Intelligence
During a major symposium, Maryellen Geiger from the University of Chicago was part of a panel exploring the use and implications of AI in imaging, with her focus on machine learning in diagnostic response. She discussed how these methods are being used to aid in compiling data on tumor characteristics, which may in turn result in the design of patient-specific diagnostics and treatments. Various AI methods are evolving as aids to radiologists as a second or concurrent reader, or as a primary autonomous reader. AI continues to look promising as an aid to assessing risk, screening, diagnosing, prognosing (based on subtypes), and predicting patient treatment response. With faster computers, larger image datasets, and advanced algorithms, we are gaining on ways to bring AI imaging into clinical practice. However, there remains to be problems with bad data, potential for misuse, lack of quantity, and the need for more field experts.
Big Data and Precision Medicine
A symposium session titled “From ‘Omics Data to Prognostic and Predictive Biomarkers” included presentations and discussion from Dr. Andrea Califano from Columbia University, Dr. Christina Curtis from Stanford University and Dr. Timothy Chan from The Cleveland Clinic. Big data and advances in data analytics can offer information for actionable use in precision medicine and health policy. Research can also be embedded into practice by gathering and aggregating data from clinical care settings. These advances may also contribute to streamlined clinical trial designs. Gathering large scale data on individual patients spanning tumor types over time is helping to generate biomarkers that can help predict individualized disease outcomes and drug responses, allowing for more precise treatment options. Pooling data aids in discovery of patterns in treatment response and predicting drug response to various tumor types, allowing for collaboration offers great benefits for research.
Barriers to collecting and assessing big data include:
- Privacy concerns
- Patient consent
- Centralizing data
- Data ownership
- Retrospective Data Analysis vs Randomized Clinical Trials
- Health disparities (populations less willing to participate)
Issues related to using clinically gathered data can include:
- Obtaining data
- Data quality
- Data accuracy
- Data reliability
- Data storage
- Data security
- Data analyses
- Need for data supplementation (tumor registry data, e.g.)
Health Equity
During the opening plenary session, Dr. Melissa Davis of Weill Cornell Medical College spoke about “Ancestry and cancer disparities: Genomic sequencing in diverse populations.” In this powerful presentation, Dr. Davis reviewed the history of forced migration as well as oncologic anthropology efforts that revealed West African ancestry and the Duffy Null allele are associated with triple negative breast cancer. Due to lack of diverse genomic information in existing large data sets, underserved populations have been systemically excluded from clinical trials and targeted therapies requiring known actionable mutations. Polyethnic-1000 is a global collaborative effort led by the New York Genome Center to collect diverse genetic information and develop race-correlated gene signatures to overcome health inequities in this area. Watch “Dr Davis Discusses Ancestry and Cancer Disparities: Genomic Sequencing in Diverse Populations” at OncLive, and read “Genomics and Cancer Disparities: The Justice and Power of Inclusion,” via Cancer Discovery.
Precision Nutrition
During the opening plenary session, Karen Vousden, PhD of the Francis Crick Institute in London, UK and Dr. Matthew Vander Heiden of Koch Institute for Integrative Cancer Research at MIT, Cambridge, MA presented “Food for thought: A conversation about the role of diet in cancer.” This fascinating discussion highlighted early work exploring the complex relationship between diet, whole body metabolism and cancer progression and the potential role of specific nutrients during cancer treatment. Work in progress suggests that differences in tumors and tumor microenvironments may need different nutritional strategies to maximize responses to different drug-based therapies. At this time, Drs. Vousden and Vander Heiden do not advocate for use of specific diets or diet/drug combinations in patients. More research is needed to inform Precision Nutrition. Watch “A Conversation About the Role of Diet in Cancer,” at The ASCO Post.