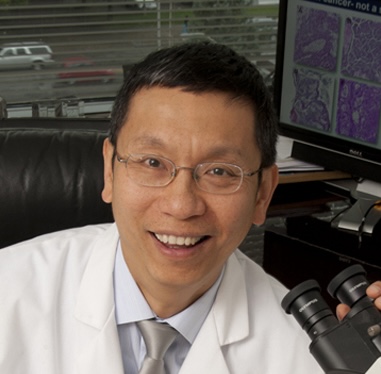
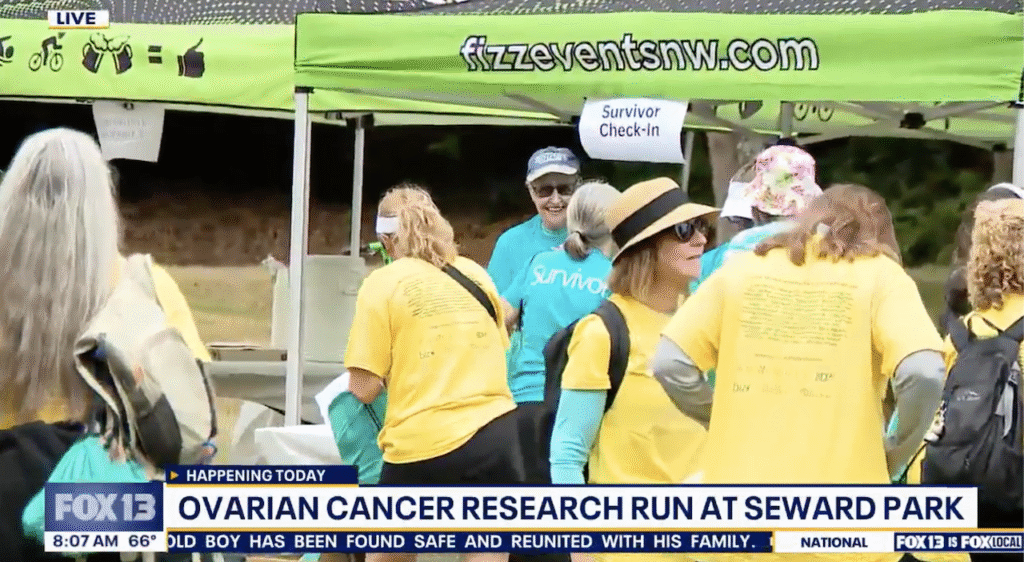
KIRO-TV 7 Seattle (CBS) Spotlights 2025 OCRA Rivkin Family SummeRun and Ovarian Cancer Research Impact
The 2025 OCRA Rivkin Family SummeRun brought together more than 900 participants in Seattle to raise critical funds for ovarian cancer research. KIRO-TV 7 Seattle (CBS) covered the event in … Continued